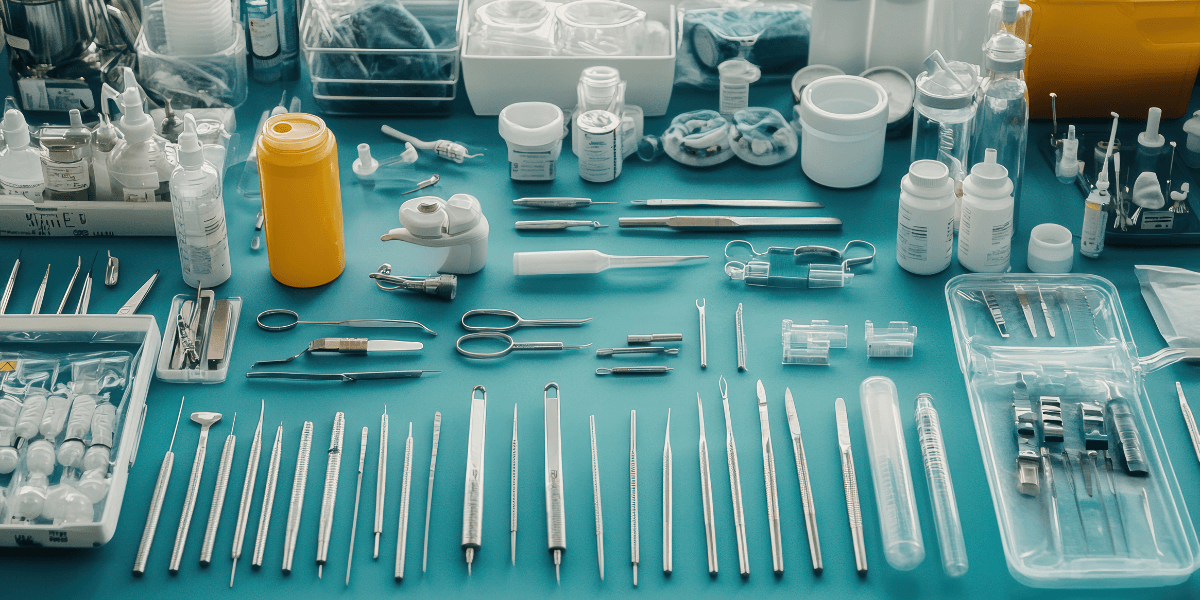
Medical instruments play a central role across diagnosis, treatment, and surgical care. Selection decisions influence hygiene standards, operational costs, workflow efficiency, and patient outcomes. Healthcare facilities frequently evaluate single-use medical instruments alongside reusable ones when planning procurement strategies. Understanding how each category functions supports informed purchasing decisions and consistent medical instrument safety practices.
Understanding Medical Instrument Categories
Medical tools fall into two primary categories based on intended lifespan. Disposable medical instruments serve one clinical procedure before disposal, while reusable tools undergo cleaning and sterilisation cycles before repeated use. Both categories support patient care across varied clinical settings.
Functional Characteristics of Single-Use Instruments
Design and Intended Use
Single-use instruments arrive pre-sterilised and ready for immediate application. These tools remove concerns around cleaning procedures, supporting streamlined clinical workflows. Many facilities rely on single-use medical instruments during emergency care, outpatient services, and high-volume clinical settings.
Infection Control Benefits
Using disposable instruments reduces cross-contamination risk. Since tools do not re-enter circulation after use, contamination transfer remains limited. This approach supports infection control objectives and strengthens medical instrument safety protocols.
Inventory and Storage Considerations
Disposable supplies require consistent stock management. Healthcare providers monitor usage closely to maintain uninterrupted availability. Storage planning becomes essential to support continuous clinical operations.
Functional Characteristics of Reusable Instruments
Durability and Construction
Reusable tools feature robust materials designed to tolerate repeated sterilisation cycles. Surgical-grade steel and reinforced polymers dominate this category. Reusable medical instruments support procedures requiring precision and structural reliability.
Sterilisation Requirements
After each use, reusable instruments undergo thorough decontamination, cleaning, and sterilisation. These steps demand trained staff, validated equipment, and strict documentation protocols to maintain compliance.
Long-Term Clinical Use
Facilities investing in reusable instruments often favour predictable performance and reduced replacement frequency. These tools support specialist procedures requiring consistent handling characteristics.
Disposable Vs Reusable Medical Instruments
In modern healthcare, the choice between disposable (single-use) and reusable medical instruments significantly influences patient safety, operational efficiency, costs, and environmental sustainability.
This balance requires careful consideration of infection risks, resource demands, and long-term impacts.
Infection Control and Patient Safety
Disposable instruments provide guaranteed sterility straight from the package, eliminating the risk of cross-contamination or improper sterilisation that can occur with reusables. Any lapse in reprocessing reusable tools may lead to healthcare-associated infections (HAIs), surgical site infections, or transmission of pathogens. Single-use options are particularly advantageous in high-risk procedures, emergency settings, or for patients with communicable diseases, enhancing overall medical instrument safety and supporting rigorous infection prevention standards.
Cost Implications
Upfront, disposable instruments often appear more expensive per unit, but they eliminate hidden costs associated with reusables, such as labour for cleaning, maintenance, repairs, replacement of damaged items, and investment in sterilisation equipment like autoclaves. Over time, reusables can offer long-term savings through repeated use, especially in high-volume settings, though unexpected downtime or failures may offset these benefits. Many hospitals adopt a hybrid approach to optimise budgets while prioritising safety.
Environmental Sustainability
Reusable instruments generate far less medical waste, reducing landfill contributions and aligning with eco-friendly healthcare goals. In contrast, single-use items contribute to substantial biomedical waste, with production, packaging, and disposal increasing greenhouse gas emissions and resource consumption. However, advancements in biodegradable materials and recycling programmes are mitigating the impact of disposables, while reprocessing reusables requires significant water, energy, and chemicals, which can offset some environmental advantages.
Performance and Consistency
Single-use instruments deliver consistent quality and sharpness for every procedure, as they are factory-fresh and free from wear. Reusables, crafted from durable materials like high-grade stainless steel or titanium, provide superior strength, precision, and customisation for complex surgeries, though repeated cycles may cause corrosion, dulling, or structural fatigue over time, potentially affecting surgeon control.
Workflow Efficiency and Convenience
Disposable instruments streamline operations by removing the need for time-consuming reprocessing, allowing staff to focus on patient care rather than decontamination. This reduces turnaround times in operating theatres and supports rapid deployment in urgent or resource-limited environments. Reusables demand structured workflows, including tracking, inventory management, and preventive maintenance, which can introduce delays if not managed effectively.
Regulatory Compliance and Traceability
Both types must meet strict standards, but disposables simplify compliance by avoiding the validation of sterilisation cycles and biological indicators required for reusables. Reprocessing protocols for reusables involve rigorous audits and documentation to ensure regulatory adherence. Single-use items reduce liability risks related to reprocessing errors, though proper disposal remains essential.
Durability and Material Quality
Reusable instruments are built for longevity, withstanding multiple sterilisation cycles without significant degradation when properly maintained. Disposables, often made from medical-grade plastics or lighter metals, prioritise functionality for one use but lack the robustness for repeated applications, making them unsuitable for highly demanding procedures.
Risk of Instrument Failure
With reusables, wear from repeated use can lead to unexpected failures during surgery, such as reduced sharpness or breakage. Disposables eliminate this concern, ensuring reliable performance each time, which is critical in precision-dependent specialties like laparoscopy or orthopaedics.
Hence, the decision hinges on procedure type, facility resources, and priorities. Disposables excel in safety and convenience, while reusables promote economy and reduced waste.
Discover high-quality medical supplies at MediTools Pty Ltd. Our medical equipment shop offers instrument trays, sterilisation containers, and trolleys designed for hygiene, efficiency, and reliable healthcare operations.
|
Aspect |
Disposable (Single-Use) Instruments |
Reusable Instruments |
|
Infection Control |
Guaranteed sterility; zero risk of cross-contamination |
Dependent on proper reprocessing; risk if sterilisation fails |
|
Patient Safety |
High, eliminates reprocessing errors |
Good when protocols followed; potential for HAIs if lapses occur |
|
Initial Cost |
Higher per unit |
Lower per unit (but requires upfront investment) |
|
Long-term Cost |
Higher overall (no reuse) |
Lower over time (multiple uses) |
|
Environmental Impact |
High waste; contributes to medical landfill and emissions |
Lower waste; more sustainable |
|
Performance Consistency |
Always fresh and sharp; uniform quality |
May dull or wear over cycles; needs maintenance |
|
Durability |
Single use only; made from lighter materials |
Built for longevity (e.g., high-grade stainless steel) |
|
Workflow Efficiency |
Fast, no cleaning required; quick turnaround |
Slower, requires decontamination, sterilisation & tracking |
|
Risk of Failure |
Very low (factory-new each time) |
Possible wear-related breakage or reduced sharpness |
Summing It Up
Selecting between single-use and reusable medical instruments requires careful consideration of safety standards, cost structures, workflow demands, and environmental impact. Both categories support modern healthcare delivery when applied appropriately. MediTools Pty Ltd supplies dependable medical instruments in Australia supporting clinical performance and regulatory compliance. Contact us for expert guidance and product support aligned with healthcare operational needs.
Disclaimer
The content provided here on the sterilization, cleaning, and reprocessing of surgical and medical instruments is strictly for informational and educational purposes only. This information is not a substitute for professional training, certification, or the manufacturer's official Instructions for Use (IFU). Sterilization is a critical, complex process that demands strict adherence to regulatory standards; improper technique can cause serious harm, including patient infection. All healthcare personnel must follow their facility's established protocols and the specific IFU for every instrument and piece of equipment. By using this blog, you agree that the author/owner holds no liability for any damages or consequences resulting from the application or misuse of this information.















